
Common skin conditions affecting the feet include Plantar Warts, Ganglion Cysts, Corns and Calluses, and Athlete’s Foot. When over-the-counter remedies don’t provide relief, medical attention is warranted.
Plantar Warts

Plantar warts (Verruca Plantaris) occur when the skin is infected by a virus, resulting in small growths on the skin.
Warts tend to appear on the bottom (plantar side) of the foot, although warts can technically develop anywhere on the foot. Plantar warts most commonly occur in the elderly, adolescents, and children.
Types of Plantar Warts
Two types of plantar warts can impact your feet.
Solitary Warts
A solitary wart is a single wart. A solitary wart often grows in size over time and may eventually multiply, forming what is known as “satellite” warts.
Mosaic Warts
Mosaic warts are clusters of multiple small warts that grow closely together, all in one area. It is more difficult to treat mosaic warts on the foot than solitary warts.
Causes of Plantar Warts
Direct contact with the human papillomavirus (HPV) causes plantar warts. HPV can also cause warts on other parts of your body.
Symptoms of Plantar Warts
If you have plantar warts, there are various symptoms you will notice, including:
Thickened Skin
People often confuse plantar warts with a callus because of the tough and thick tissue that develops.
Tiny Black Dots
If you look closely at the surface of the plantar wart, you will see tiny black dots. These tiny black dots are dried blood contained in the capillaries (tiny blood vessels). They appear on the surface of the wart.
Pain
If you squeeze the side of the wart, you may feel pain. Walking and standing may also be painful.
Plantar warts start small and become bigger over time, growing deep into your skin. This growth occurs over time.
Treatment for Plantar Warts
Over time, plantar warts can clear up on their own. However, for faster treatment, Dr. Wawrzynek may use Swift treatment, prescribe topical or oral medications or surgery to remove warts. The goal of any treatment is to remove the wart completely.
Ganglion Cysts
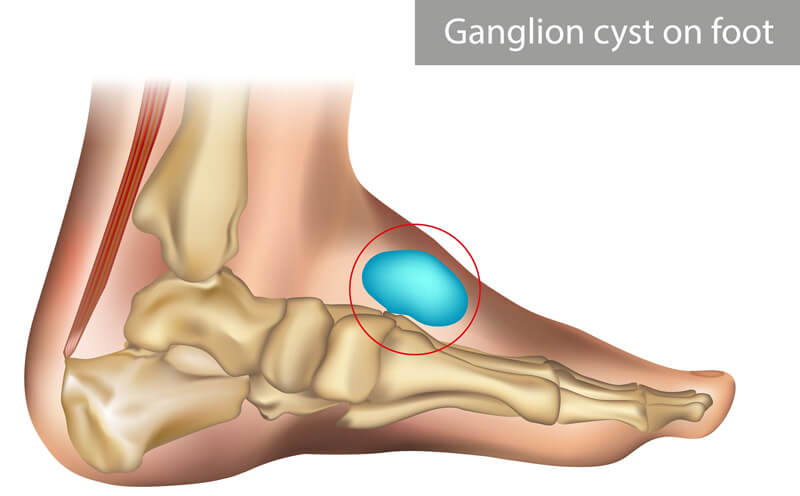
Ganglion cysts are small sacs of fluid that form near joints and tendons in the foot. The fluid is a thick, sticky, clear, jelly-like material.
Causes of Ganglion Cysts on the Feet
An outpouching of synovial fluid causes a ganglion cyst. This fluid comes from a tendon or joint protruding toward the skin’s surface. Ganglion cysts develop from repetitive microtrauma, although they can also occur due to a single traumatic event.
Ganglion cysts are generally non-painful and don’t require medical treatment. However, if they are applying pressure to nearby structures, you will need medical treatment.
Symptoms of Ganglion Cysts on the Feet
Ganglion cysts are generally soft and don’t move. They appear as bumps that change in size from 1 to 3 cm in diameter.
Cysts often make it difficult to wear shoes because the shoes rub against the bumps. If cysts touch nerves, you may feel a tingling or burning sensation.
Diagnosing Ganglion Cysts
During your examination, Dr. Wawrzynek will press on the lump to see if it is moveable. She may also remove a small amount of fluid for evaluation. In certain situations, she may order x-rays and other imaging studies to confirm the diagnosis.
Treatment for Ganglion Cysts
Treatment for ganglion cysts includes non-surgical and surgical options, some of which include:
- Monitoring the cyst, but no treatment, especially if they aren’t causing any pain or discomfort.
- Recommending you wear different shoes that don’t rub or irritate the cyst or placing a pad inside the shoe to reduce any pressure against the cyst.
- Draining the fluid and injecting a steroid medication into the mass.
If non-surgical treatment options are ineffective and the cyst keeps growing, Dr. Wawrzynek may recommend surgical removal of the cyst.
Corns and Calluses

Corns are a buildup of hard dead skin that form cone-like bumps on the toes due to repetitive pressure and friction caused by repetitive activities like running, climbing stairs, and skiing. Bunions and hammertoes may also cause corns on the feet.
Calluses are thick, hard skin that generally forms on the sides and balls of the feet or the heels. Calluses form as the result of repetitive friction and pressure on your feet from shoes, sports, daily activities, or the way you walk. Keratinocytes, special skin cells in the outer layer of your skin, produce calluses.
For painful seed corns or porokeratomas, Swift treatment can be an effective way to relieve the issue. One of the best ways to heal corns and calluses is to wear shoes that fit properly and provide you with ample support in the toe box. Wearing properly fitting shoes will help take the pressure off your corns or calluses and they may go away on their own. If they heal, call Dr. Wawrzynek to discuss treatment options.
Athlete’s Foot

Athlete’s foot is a common fungal infection. The infection impacts the upper layers of the skin of the foot and usually starts between the toes, but it can also develop along the soles, arches, and sides of the feet.
Athlete’s foot is contagious. It can easily spread in public places where the conditions are warm and moist and where people tend to walk around barefoot, such as in locker rooms, showers, and indoor and outdoor swimming pools.
The Cause of Athlete’s Foot
Trichophyton causes athlete’s foot. The fungus is commonly found in clothing and on floors.
Just like other fungi, Trichophyton thrives when in damp and warm conditions. If you wear thick shoes that tightly squeeze your toes together, or if you wear damp socks on warm feet, the chances of developing athlete’s foot increase.
The Symptoms of Athlete’s Foot
Symptoms of Athlete’s foot include:
- Blisters
- Pain
- Itching
- Stinging
- Scaly rash
- Flaking of the skin
- Burning sensation
- Inflammation
- Redness between the toes
- Scaling between the toes
Diagnosing Athlete’s Foot
Dr. Wawrzynek uses a skin potassium hydroxide test to scrape a sample of infected tissue and places it under potassium hydroxide (KOH). The KOH solution destroys human cells, leaving only the fungal cells.
Treatment for Athlete’s Foot
Treatment for Athlete’s foot depends on the severity of the condition. If it is a mild condition, you can use over-the-counter medications. For more severe cases, Dr. Wawrzynek prescribes a more powerful antifungal medication.
If Athlete’s foot is left untreated, the symptoms can spread from toe to toe or to a nail and cause a fungal nail infection.
Preventing Athlete’s Foot
Follow these tips to help prevent athlete’s foot:
- Wear footwear made of breathable materials that allow air to circulate around the feet.
- Wash and dry feet thoroughly, even between the toes.
- Use powder to keep the feet dry.
- Change socks several times daily.
- Keep socks and footwear clean and dry.
- Never share socks or footwear.
- Avoid constrictive footwear, stockings, and socks, as they can trap moisture and perspiration on the feet.
- Wear flip-flops or shower shoes in public areas such as showers, pools, and locker rooms. Don’t walk barefoot around these areas.
Dr. Melissa Will Help Get You Back On Your Feet
Dr. Melissa Wawrzynek is a board-certified foot and ankle specialist and offers a broad range of advanced orthopedic, sports medicine, and regenerative treatments.
Our doctor and her team will consult with you regularly to ensure you return to health and receive the highest quality care.
If you’re ready to return to full speed as quickly, easily, and safely as possible, schedule an appointment today.

